



Epidemiology
0.2% of all orthopedic injuries
Mechanism
High energy
Fracture dislocation of the tarso-metatarsal (TMT) joints
| Twisting / abduction injury of forefoot | Axial Loading | Direct Crush |
|---|---|---|
|
MVA |
Fall from height |
Risk compartment syndrome Open fractures |
Classification
| Isolated | Homolateral | Divergent |
|---|---|---|
| Only 1st MT injured / displaced | All 5 metatarsals displaced in same direction |
1st metatarsal displaces medially Other 4 metatarsals displace laterally |
| Most common | Least common | |
 |
 |
 |
Anatomy
Bony Stability
| Alignment | Alignment | Roman arch | Keystone / Mortise |
|---|---|---|---|
|
1st metatarsal - medial cuneiform 2nd metatarsal - middle cuneiform 3rd metatarsal - lateral cuneiform
AP foot view |
4th and 5th metatarsals articulate with cuboid
Oblique foot view |
Bases of metatarsal wider dorsally than plantar Form half of Roman arch |
2nd metatarsal is keystone of transverse metatarsal arch - middle cuneiform is recessed proximally - mortise provided for base of second metatarsal |
 |
 |
 |
 |
Ligamentous stability
| LisFranc Ligament | Interosseous cuneiform ligaments | Tarso-metatarsal joints | Inter-metatarsal ligaments |
|---|---|---|---|
| Plantar, interosseous and dorsal | Plantar, interosseous and dorsal | Plantar and dorsal | Plantar, interosseous and dorsal |
| Base of 2nd metatarsal to medial cuneiform | Medial to intermediate cuneiform | Tarsometatarsal ligamaments | Metatarsal bases |
| Plantar most important | Plantar strongest | Plantar stronger - usually displace dorsally | No connection between 1st and 2nd metatarsal |
Examination
Significant swelling and pain
Bruising plantar aspect foot indicative of Lis Franc ligament rupture
Signs compartment syndrome
Compound wounds

Injury patterns
Lisfranc ligament - medial cuneiform - 2nd metatarsal
Inter-cuneiform ligament - medial cuneiform (C1) - middle cuneiform (C2) widening
1st TMT joint dislocation - medial cuneiform (C1) - 1st metatarsal
2nd TMT joint dislocation - middle cuneiform (C2) - 2nd metatarsal
3rd TMT joint dislocation - lateral - cuneiform (C3) - 3rd metatarsal
4th & 5th TMT joint dislocation - cuboid to 4th & 5th metatarsal
Imaging
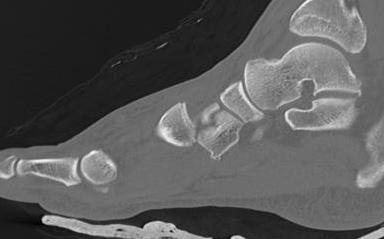
1. Diastasis of the intermetatarsal gap between the 1st and 2nd metatarsals
2. Widening of the space between the medial cuneiform and base of 2nd metatarsal
3. Second metatarsal Fleck sign - avulsion of Lisfranc ligament from base of 2nd metatarsal
4. Widening of inter-cuneiform distance
5. Dorsal subluxation of the metatarsals
6. Tarsometatarsal alignment disruption
- medial border 1st metatarsal aligns with medial border medial cuneirform (AP foot)
- medial border 2nd metatarsal aligns with medial border middle cuneiform (AP foot)
- medial border 3rd metatarsal aligns with medial border lateral cuneiform (AP view)
- medial border 4th metatarsal aligns with medial border of the cuboid (oblique view)
X-ray
AP / Assess medial column


Internal Oblique 30o / Assess lateral column



Lateral / assess dorsal displacement


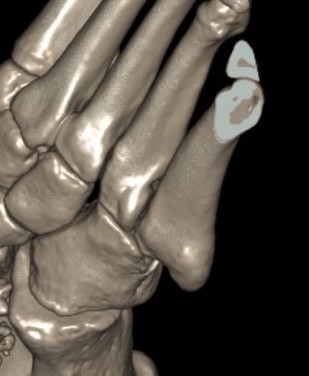
CT scan





Dorsal displacement of metatarsals
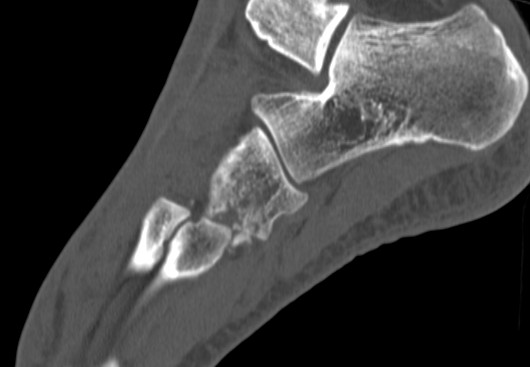
Compression fractures / nutcracker of cuboid
Operative Management
Indications
Any displacement
Options
1st, 2nd & 3rd TMT joints
- trans-articular screw fixation
- bridge plate fixation
- primary arthrodesis
4th & 5th TMT joints
- consider K wire fixation
Results
Primary arthrodesis
MacTier et al Foot Ankle Orthop 2024
- meta-analysis of 5 RCTs and 240 patients
- ORIF versus primary arthrodesis
- better pain scores and patient satisfaction at 2 years with primary arthrodesis
Bridge plating versus transarticular screws
Philpott et al J Foot Ankle Surg 2021
- systematic review bridge plating compared to trans-articular screws
- 17 studies and 450 patients
- better outcomes with bridge plating compared to trans-articular screws
1st TMT
- 78 patients with 1st TMT dislocation and Lis Franc
- ORIF versus primary arthrodesis
- improved functional outcomes with arthrodesis
- loss of reduction in 25% of ORIF
Stodle et al Foot Ankle Int 2020
- Lis Franc with 1st tarsometatarsal dislocation
- RCT of temporary plate fixation versus arthrodesis
- 48 patients
- no difference in outcome at 2 years
Timing
Wait for swelling to reduce
2 - 3 weeks
Two Incision Approach
First dorsal incision between 1st and 2nd metatarsal
- protect branches of superficial peroneal nerve
- retract EHL medially
- dorsalis pedis and deep peroneal nerve are in this intermetatarsal space
Second dorsal incision between 3rd and 4th metatarsal
Technique
AO foundation surgical approach Lisfranc
Vumedi LisFranc Fracture ORIF video
Reduction
- medial incision over medial cuneiform
- clamp medial cuneiform to base 2nd metatarsal
AP view
- 1st metatarsal to medial cuneiform
- 2nd metatarsal to intermediate cuneiform
- medial cuneiform to base of second metatarsal / Lisfranc joint
- medial cuneiform to intermediate cuneiform / inter-cuneiform joint
Oblique view
- 3rd metarsal to lateral cuneiform
- 4th metatarsal to cuboid
- 5th metatarsal to cuboid

Screw fixation 1st and 2nd TMT with K wire fixation 3rd / 4th / 5th


Bridge plating of 1st, 2nd, 3rd & 4th TMT with screw fixation of Lisfranc joint


Fusion of 1st TMT, plating of 2nd and 3rd TMT, K wire stabilization of 4th and 5th TMT
Removal of metalwork
Rhodes et al Foot Ankle Orthop 2022
- systematic review of 28 studies and 1000 patients
- minimal improvement in functional outcome with implant removal
Complications
Deep infection
Painful metalwork
Midfoot osteoarthritis
Sinkler et al J Orthop Trauma 2024
- 118 patients with Lisfranc fracture dislocations
- Level 1 trauma center
- 23% open fractures
- removal of implants 26%
- deep infection 8%
- post traumatic osteoarthritis 37%
